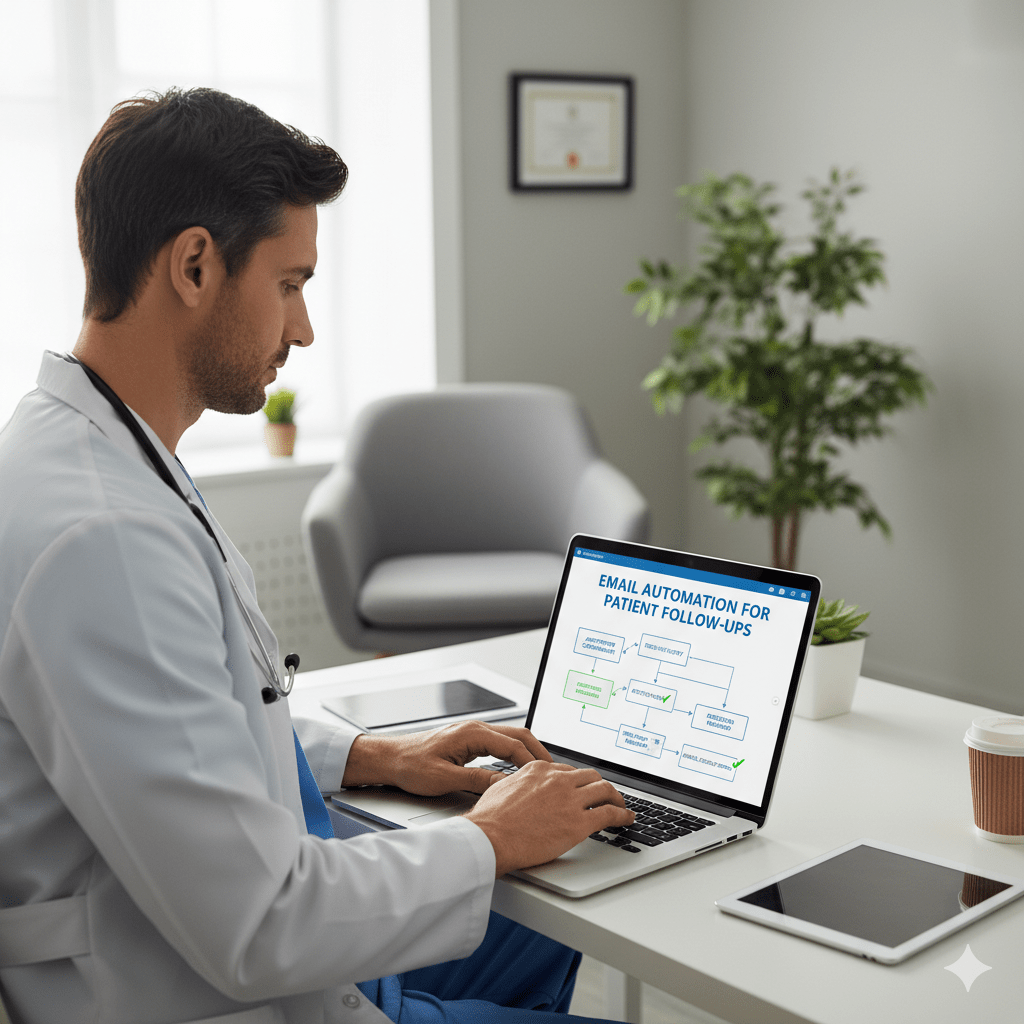
“Use multi-step, HIPAA-compliant workflows to reduce no-shows by reinforcing appointments, making Email Automation for Patient Follow-Ups essential.”
That empty slot in your schedule. You know the one. It was supposed to be a new patient consultation or a crucial follow-up. Your staff prepped the room. The physician reviewed the chart. And then… nothing. The patient never arrived. No call, no email, just a gaping hole in the day’s revenue and a disruption to the finely tuned rhythm of your practice. This isn’t just an occasional annoyance; it’s a chronic, costly problem. Patient no-shows drain resources, delay care for others, and have a direct impact on your bottom line.
On the other side of the coin is the post-appointment communication gap. A patient leaves your office with a head full of new information—medication instructions, follow-up requirements, and lifestyle changes. But life gets in the way. Instructions are forgotten, prescriptions go unfilled, and what should have been a straightforward path to better health becomes a series of missed opportunities. Both of these challenges—costly no-shows and inconsistent follow-up—stem from the exact root cause: a communication breakdown.
The traditional solution of making manual phone calls and sending one-off emails is no longer sufficient. Your front desk staff are heroes, but they can’t be everywhere at once. They’re juggling check-ins, billing questions, and ringing phones. It’s an unsustainable model in a world where patients expect seamless, digital communication.
Fortunately, there’s a powerful and practical solution. This guide will provide a comprehensive overview of how your practice can effectively implement email automation for patient follow-ups and other critical communications. We’ll explore how to build automated workflows that not only dramatically reduce patient no-shows but also create a more consistent, supportive, and effective care journey for every patient. This isn’t about replacing your team with robots; it’s about equipping them with intelligent tools to enhance efficiency, increase revenue, and, most importantly, deliver better care.
The Crushing Weight of an Empty Chair: Understanding the True Cost of No-Shows
When a patient fails to show up for an appointment, the most obvious impact is financial. If a single appointment slot generates $150 in revenue and you have just two no-shows per day, that’s $300 in lost revenue per day. Over a month, that’s thousands of dollars. Over the course of a year, it could be equivalent to a staff member’s salary. However, the damage extends far beyond the immediate loss of revenue. The ripple effects of a no-show disrupt your entire practice.
The Financial Domino Effect
The direct loss is only the beginning. Consider the sunk costs associated with that appointment slot. Your staff spent time preparing for the patient’s arrival—pulling charts, verifying insurance, and prepping the examination room. The physician may have spent time reviewing the patient’s history. These are all billable hours that produced zero return.
Furthermore, that empty slot represents a lost opportunity. Another patient, who was waiting for an opening, could have taken that spot, received necessary care, and generated revenue. Last-minute openings are notoriously difficult to fill, meaning the loss is rarely recouped. This persistent financial drain can hinder your practice’s ability to invest in new equipment, training, or staff, ultimately stunting its growth.
The Operational Quicksand
A no-show throws a wrench into the day’s carefully planned schedule. It creates an awkward gap that can either lead to unproductive downtime or a frantic scramble to pull a waiting patient forward, which then disrupts the flow for everyone else. This unpredictability is a significant source of stress for your front desk and clinical teams. They are constantly reacting, trying to patch the holes in a schedule that should run smoothly.
Think about the administrative labor involved. After the no-show, a staff member likely has to:
- Update the patient’s record with the “no-show” status.
- Attempt to contact the patient to understand why they missed the appointment.
- Try to reschedule the appointment, which involves another round of phone calls or messages.
- Manage the cancellation policy, if applicable, which can lead to uncomfortable financial conversations.
Each of these steps pulls your team away from higher-value tasks, such as assisting patients who are physically present in your office or handling complex insurance inquiries. It’s a classic case of working in the practice instead of on the practice.
The Unseen Clinical Consequences
The most serious impact of a no-show is on the patient’s health. A missed appointment is a missed opportunity for care. For a patient with a chronic condition like diabetes or hypertension, a missed check-up can mean a failure to adjust medications, leading to poor disease management and potential complications down the line. For a patient awaiting a diagnosis, it means a delay in starting a potentially life-altering treatment. For someone scheduled for a post-operative follow-up, it could mean a surgical site infection goes unnoticed.
These lapses in care not only harm the patient but also expose the practice to potential liability. Consistent follow-up and monitoring are pillars of quality healthcare. When patients repeatedly miss appointments, it fragments their care history. It makes it incredibly difficult for providers to maintain a comprehensive overview of their health, ultimately compromising patient compliance and outcomes.
Why Your Manual Follow-Up System is Failing
For decades, the telephone has been the primary tool for patient reminders. Your front desk staff diligently work their way through tomorrow’s appointment list, dialing numbers, leaving voicemails, and hoping for a call back. While the intention is noble, this manual process is fundamentally broken in the modern healthcare environment. It’s inefficient, inconsistent, and fails to meet the expectations of today’s digitally-savvy patients.
The simple reality is that your staff’s time is one of your most valuable resources. Every minute an employee spends on the phone leaving a reminder voicemail is a minute they are not helping a patient at the check-in counter, resolving a billing issue, or managing prior authorizations. The task is repetitive and time-consuming. Consider the workflow: dial number, wait for an answer, deliver the message (or leave a voicemail), hang up, document the call, repeat. This process can consume hours each day—hours that could be redirected toward tasks that require a human touch and critical thinking.
Moreover, this manual system is inherently prone to human error. A busy afternoon, an unexpected staff absence, or a sudden influx of patients can easily lead to missed calls. Reminders may be sent too late. The messaging can be inconsistent; one staff member might remember to mention the cancellation policy, while another forgets. This lack of standardization creates a disjointed patient experience, leading to confusion and frustration.
The biggest issue, however, is that this system simply isn’t scalable. As your practice grows and your patient volume increases, the manual reminder system collapses under its own weight. You can’t simply ask your staff to make more calls; their time is finite. This creates a ceiling for your practice’s efficiency and growth. You’re forced to choose between thorough patient communication and managing the day-to-day operations of the office, a choice no practice should have to make. Ultimately, relying on manual calls is like trying to fill a swimming pool with a teaspoon—the effort is immense, and the results are underwhelming.
The Automation Revolution: Your New Frontline Against No-Shows
Imagine a system that works tirelessly in the background, 24/7. It never calls in sick, never forgets a task, and executes every communication with perfect consistency. This is the power of healthcare workflow automation. It’s not about removing the human element; it’s about automating the repetitive, predictable tasks so your human team can focus on what they do best: caring for patients. When it comes to no-shows, automated appointment reminders are your single most effective weapon.
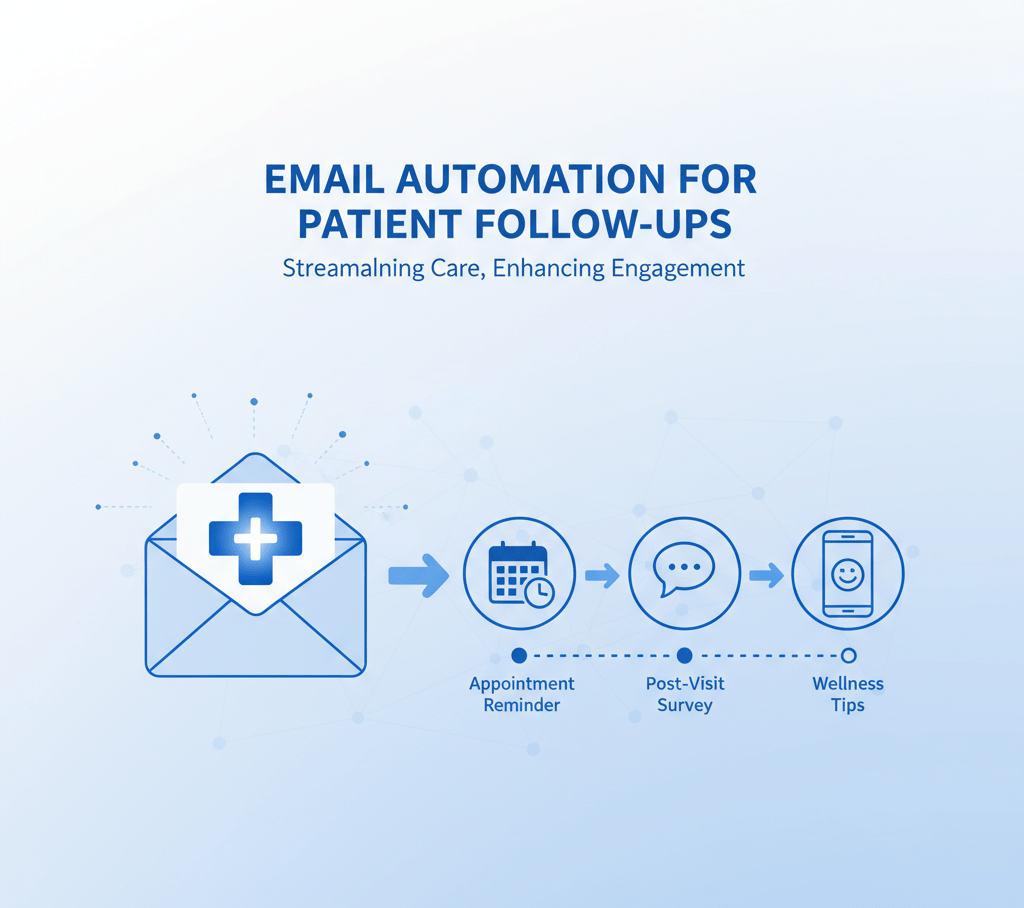
A well-designed automated reminder sequence is more than just a single email. It’s a strategic series of communications designed to keep the appointment top-of-mind and make it incredibly easy for patients to confirm or reschedule their appointment.
The Anatomy of a Perfect Reminder Sequence
Let’s break down what a highly effective, multi-step reminder workflow looks like.
1. The Instant Confirmation (Sent immediately upon booking)
- What It Is: As soon as your staff books an appointment in your practice management software, the system automatically triggers an email to the patient.
- Why It Works: This provides immediate reassurance. The patient is aware that the appointment is confirmed and all details are accurate. It eliminates the uncertainty that can lead to a patient forgetting they even made the appointment.
- Essential Content:
- Clear Subject Line: “Appointment Confirmed: Your Visit with Dr. Evans on October 28th”
- Personalization: “Dear [Patient First Name],”
- Key Details: Date, Time, Physician Name, and Practice Location/Address.
- The Magic Button: Include a prominent “Add to Calendar” link that works for Google Calendar, Outlook, and Apple iCal. This simple feature significantly increases the likelihood that the appointment is added to their personal schedule.
2. The Gentle Nudge (Sent 7 days before the appointment)
- What It Is: A friendly, low-pressure reminder sent a whole week in advance.
- Why It Works: A lot can happen in a week. This email serves as a crucial checkpoint. It gives patients ample time to recognize a conflict that has arisen—a work meeting, a child’s school event—and reschedule without penalty. This is your best opportunity to open up that slot for another patient.
- Essential Content:
- Reiterate all the key appointment details.
- Include clear links or phone numbers for rescheduling. Frame it positively: “If your plans have changed, you can easily reschedule by clicking here or calling our office.”
- This is a great place to add value—link to any pre-visit forms that can be filled out online to save time during check-in.
3. The Critical Confirmation (Sent 48-72 hours before the appointment)
- What It Is: This is the most crucial message in the sequence. It’s not just a reminder; it’s a call to action.
- Why It Works: This email explicitly requests that the patient confirm their attendance. It forces a response that provides you with actionable data. When a patient clicks “Confirm,” their appointment status in your scheduler can be automatically updated. If they click “Cancel” or “Reschedule,” your front desk is immediately alerted to an opening.
- Essential Content:
- Action-Oriented Subject Line: “Please Confirm Your Upcoming Appointment”
- Clear, Bold Buttons: [CONFIRM APPOINTMENT] [RESCHEDULE]
- A polite but firm reminder of your cancellation policy: “Please note that a fee may be charged for cancellations made less than 24 hours in advance.” This simple sentence adds weight to the confirmation request.
4. The Day-Of Lifesaver (Sent the morning of the appointment)
- What It Is: A final, brief reminder sent a few hours before the scheduled time. While this can be an email, it’s often most effective as an SMS text message for its immediacy.
- Why It Works: This message foils the most common reason for a no-show: simple forgetfulness. It cuts through the noise of a busy day and puts the appointment front and center right when it matters most.
- Essential Content:
- Keep it short and sweet. “Hi [Patient First Name], this is a reminder of your appointment today at 2:30 PM with Dr. Evans. Our address is 123 Main St. We look forward to seeing you!”
- Including a link to Google Maps for directions is a beneficial touch that removes one more potential barrier to arrival.
This multi-step, multi-channel approach covers all the bases. It provides convenience for the patient and invaluable, actionable data for your practice, transforming your scheduling from a reactive, guesswork-based system into a proactive and efficient one.
Beyond Reminders: Improving Care with Pre- and Post-Visit Automation
Reducing no-shows is a massive win, but it’s only half the battle. True practice management excellence involves creating a seamless patient journey that extends before they arrive and long after they leave. Automation is the key to delivering this consistent, high-quality experience at scale, directly contributing to better patient compliance and satisfaction.
Setting the Stage for Success: Automated Pre-Visit Instructions
How often do patients show up for a procedure unprepared? They forgot to fast, didn’t arrange for a ride home, or failed to stop taking a specific medication. These situations cause frustrating delays, last-minute cancellations, and can even pose a risk to patient safety.
Automated pre-visit workflows, triggered by the specific appointment type, can virtually eliminate these problems.
Let’s imagine a workflow for a patient, Sarah, scheduled for a routine colonoscopy:
- Trigger: An appointment has been booked with the type “Colonoscopy” in your PMS.
- Email 1 (Sent 10 days prior): “Getting Ready for Your Upcoming Colonoscopy”
- This initial email provides a high-level overview of the project. It explains the importance of the preparation, provides a shopping list for the required prep kit, and details any dietary modifications she needs to make in the coming days. It may also include a link to an educational video on your website that provides a more detailed explanation of the procedure.
- Email 2 (Sent 3 days prior): “Your Colonoscopy Prep Instructions”
- This is the detailed, step-by-step guide. It outlines the clear liquid diet, gives the exact times to start drinking the prep solution, and offers tips for making the process more tolerable. By delivering this information digitally, Sarah can easily refer to it on her phone or computer instead of trying to find a misplaced paper handout.
- Email 3 (Sent 1 day prior): “Final Checklist for Your Procedure Tomorrow”
- This is a final confirmation and checklist. “Remember: nothing to eat or drink after midnight. Have you confirmed your ride home? Please bring your insurance card and photo ID.” This simple checklist minimizes patient anxiety and ensures all logistical details are handled.
By the time Sarah arrives, she is fully prepared, confident, and knows exactly what to expect. This improves clinical outcomes, reduces her anxiety, and keeps your schedule running like clockwork. This level of proactive care is nearly impossible to deliver consistently with a manual process.
Closing the Loop: The Power of Post-Appointment Follow-Up
The time immediately following a medical appointment is critical. This is when patients can feel adrift, trying to recall the doctor’s instructions amidst the flurry of daily life. Email automation for patient follow-ups bridges this gap, reinforcing your guidance and demonstrating to patients that your commitment to their health doesn’t end when they leave the office. This is a cornerstone of effective patient retention strategies.
Workflow 1: The Immediate Visit Summary (Sent 1-2 hours after checkout)
- As soon as a patient’s appointment is marked as “complete,” an email is sent.
- Subject: “A Summary of Your Visit with Dr. Evans Today”
- Content: It starts with a warm “Thank you for visiting us today.” It then provides a clear, bulleted list of the most important takeaways:
- “Take Amoxicillin 500mg twice daily for 7 days.”
- “Schedule a follow-up appointment in 4 weeks.”
- “Please log in to our secure Patient Portal for your complete visit notes.”
- Impact: This simple email serves as a written reinforcement of all the discussed points, significantly improving medication adherence and compliance with the treatment plan.
Workflow 2: The Proactive Check-In (Sent 3-4 days after a new prescription)
- This workflow is triggered when a new medication is added to the patient’s chart.
- Subject: “A quick check-in from [Your Practice Name]”
- Content: “Hi [Patient First Name], we’re just following up to make sure you were able to pick up your new prescription from the pharmacy. If you have any questions about how to take it or are experiencing any side effects, please call our office right away.”
- Impact: This one email can be compelling. It can identify potential adverse reactions early, address barriers to filling the prescription (such as cost or pharmacy issues), and make the patient feel genuinely cared for.
Workflow 3: The Strategic Feedback & Review Request (Sent 24 hours after visit)
- This workflow is your key to managing and building your online reputation.
- Subject: “How did we do? Tell us about your visit.”
- Content: The email asks for direct feedback first. “Your opinion is vital to us. On a scale of 1-5, how would you rate your recent experience?”
- The Smart Logic: This is where the automation gets brilliant.
- If the patient clicks 4 or 5 stars, they are taken to a thank-you page that says, “We’re thrilled you had a positive experience! People in our community rely on reviews to find great care. Would you be willing to share your feedback publicly on Google?” It then provides a direct link to your Google Business Profile review page.
- If the patient clicks 1, 2, or 3 stars, they are taken to a different page. This one says, “We are so sorry that we did not meet your expectations. Your feedback is being sent directly to our practice manager, who will be in contact with you shortly to learn more about how we can improve.”
- Impact: This system directs satisfied patients to public review sites, systematically enhancing your online reputation. Simultaneously, it captures negative feedback internally, providing you with a priceless opportunity to perform service recovery and address underlying operational issues before they escalate into public complaints.
The Technical Details: Choosing HIPAA-Compliant and Effective Tools
Venturing into the world of patient communication automation requires careful attention to one critical factor: security. The Health Insurance Portability and Accountability Act (HIPAA) governs the handling of patient information, and the penalties for non-compliance are severe. This is not an area where you can afford to cut corners.
HIPAA Compliance is Absolutely Non-Negotiable
Standard email marketing platforms, such as Mailchimp, Constant Contact, or ConvertKit, are not suitable for this purpose. They are not designed to handle Protected Health Information (PHI). Sending an email that says, “Hi John Smith, this is a reminder of your appointment with Dr. Evans for your diabetes check-up,” contains multiple pieces of PHI and would be a HIPAA violation if sent through a non-compliant service.
To operate legally and ethically, any software vendor you use must be willing to sign a Business Associate Agreement (BAA). A BAA is a legally binding contract that requires the vendor to uphold the same rigorous standards of PHI protection that your practice does. If a company won’t sign a BAA, you absolutely cannot use them for patient communications.
Key Features to Look for in a Patient Communication Platform
When evaluating different patient communication tools or practice management software add-ons, look beyond the basic features. Here’s what truly matters:
- Deep Integration with Your PMS/EHR: This is the most critical technical feature. The automation platform must be able to communicate directly with your Practice Management Software or Electronic Health Record system (e.g., Epic, Cerner, Athenahealth, eClinicalWorks, etc.). The workflows we’ve discussed are only truly “automated” if they are triggered by events in your schedule—a new appointment booked, a status changed to “checked-out.” Manually exporting lists of patients and uploading them to another system every day defeats the entire purpose of automation and introduces opportunities for error.
- Workflow Customization and Segmentation: A one-size-fits-all approach doesn’t work. You need the ability to build custom logic. For example, send a different reminder sequence to new patients than you do to established ones. You need to be able to trigger specific pre-procedure instructions based on the type of appointment. The ability to segment your patient list (e.g., “send this educational email to all diabetic patients who haven’t been seen in 6 months”) is a hallmark of a robust system.
- Multi-Channel Capabilities: Although this guide primarily focuses on email automation for patient follow-ups, the ideal platform should offer an integrated, multi-channel approach. The ability to send SMS text messages for urgent, day-of reminders is incredibly effective. Some platforms also provide automated voice calls or secure patient portal messaging, allowing you to meet patients where they are most comfortable.
- Robust Analytics and Reporting: How do you know if your efforts are working? Your platform should provide clear, easy-to-understand dashboards. You need to be able to track email open rates, click-through rates on confirmation links, and the number of reviews generated. This data is essential for measuring your return on investment and optimizing your communication strategies over time.
Your Step-by-Step Implementation Guide
Adopting a new technology can seem intimidating, but by breaking it down into manageable steps, you can ensure a smooth and successful transition.
Step 1: Audit Your Current Communication Chaos. Before you can build a better future, you need to understand your present. Sit down with your team and map out your current processes. How are you currently reminding patients? Who is responsible? How much time does it take? Where are the most common points of failure? This honest assessment will highlight the areas where automation can have the most immediate impact.
Step 2: Define Your Specific, Measurable Goals. What does success look like for your practice? Don’t just say “we want fewer no-shows.” Get specific. “We want to reduce our no-show rate from 15% to below 8% within six months,” or “We want to generate 20 new 5-star Google reviews per month.” Having clear, quantifiable goals will help you focus your efforts and measure your success.
Step 3: Research and Select Your Technology Partner Using the criteria outlined in the previous section (HIPAA compliance, PMS integration, etc.), begin researching potential vendors. Schedule demos with your top 2-3 choices. Involve your office manager and front desk lead in these demos—they are the ones who will be using the system on a day-to-day basis, and their buy-in is crucial. Don’t be afraid to ask tough questions about their integration process, training, and customer support.
Step 4: Design Your Foundational Workflows. Start simple. Don’t try to automate everything on day one. The single best place to begin is with the automated appointment reminder sequence. It provides the fastest and most easily measurable return on investment. Write the actual copy for each email in the sequence. Keep the language clear, friendly, and professional. Map out the timing and triggers for each message.
Step 5: Train Your Team and Prepare for Launch. Technology is only a tool; your people make it work. Hold a dedicated training session for your staff. They need to understand how the system works, what the emails contain, and how to respond to patient questions about the new reminders. Empower them to see the system as their assistant, a tool that frees them from tedious tasks and allows them to provide better service to the patients in front of them.
Step 6: Go Live, Monitor, and Optimize. Launch your first workflow. For the first few weeks, keep a close eye on the analytics. Are patients opening the emails? Are they clicking the “Confirm” button? If your open rates are low, try A/B testing different subject lines. If confirmation rates are low, make the buttons in your email larger and more prominent. Continuous, data-driven optimization is the key to long-term success.
The Human Touch: Why Automation Enhances, Not Replaces, Your Team
A common fear is that automation will make your practice feel cold, corporate, and impersonal. In reality, the opposite is true. When implemented thoughtfully, automation elevates the human connection in your practice.
Think about your front desk staff right now. How much of their day is spent on repetitive, low-value communication? Leaving voicemails, repeating the exact pre-visit instructions over and over, chasing down appointment confirmations. Now, imagine if all of that were handled automatically.
Suddenly, your team is free. They are free to make genuine eye contact with the anxious patient in the waiting room. They have the time to explain a complex insurance statement to a confused senior carefully. They have the mental bandwidth to greet every person who walks through the door with a warm, unhurried smile.
Automation handles the routine tasks, allowing your team to focus on the exceptions. It manages the predictable so your people can manage the personal. A well-written, personalized email that arrives at the perfect time feels attentive and professional. A rushed, distracted phone call from a staff member trying to do five things at once does not. By taking the administrative burden off your team, you empower them to be the compassionate, caring heart of your practice.
Streamline Your Practice, Enhance Your Care with InvigoMedia
We’ve covered the why and the how. You now understand the profound impact that a smart automation strategy can have on your practice, from stabilizing your revenue by reducing no-shows to improving patient outcomes through consistent follow-up. You see the path from operational chaos to streamlined efficiency.
But we also understand that you are a healthcare provider, not a software integration specialist or a digital marketing expert. The prospect of vetting HIPAA-compliant vendors, designing complex workflows, and writing compelling email copy can feel overwhelming. That’s precisely where InvigoMedia comes in.
We are more than just a marketing agency; we are a strategic partner for medical practices looking to thrive in the digital age. We specialize in bridging the gap between your clinical expertise and the powerful patient communication tools that can transform your practice.
Our team works with you to:
- Select the Right Platform: We help you navigate the complex market of HIPAA-compliant email automation tools to find the perfect fit for your practice’s specific needs and budget.
- Ensure Seamless Integration: We manage the technical heavy lifting, working with your team and your PMS/EHR vendor to ensure your new system communicates flawlessly with your existing software.
- Design and Build Expert Workflows: We leverage our experience and industry best practices to design, write, and implement high-impact automated sequences—from appointment reminders to review generation.
- Provide Ongoing Management and Optimization: We don’t just set it and forget it. We continuously monitor your analytics, provide you with clear reports on your progress, and work with you to refine your strategy over time.
You are committed to delivering the highest quality care to your patients. Let us handle the communication framework that supports that mission. Stop letting no-shows dictate your daily revenue and start building a more resilient, efficient, and patient-centric practice.
Ready to see how automation can work for you? Contact InvigoMedia today for a free, no-obligation consultation. Let’s build a better communication system for your practice, together.
Frequently Asked Questions (FAQs)
Q1: Is email automation for patient communication really HIPAA compliant?
Yes, absolutely, provided it is done correctly. The key is using a software platform specifically designed for the healthcare industry and willing to sign a Business Associate Agreement (BAA) with your practice. This agreement legally binds them to protect all PHI. Standard marketing platforms are not compliant; however, dozens of excellent, secure, and HIPAA-compliant options are available.
Q2: A lot of my patients are older. Will they even check their email for reminders?
This is a common concern, but data shows that technology adoption among seniors is higher than ever. A multi-channel approach is key. While email is the foundation, the best systems also integrate SMS text messages, which have incredibly high open rates across all age groups. Automation doesn’t entirely replace traditional methods; it simply enhances them. You can still have your staff make targeted phone calls to patients who are known to be less tech-savvy, while the system handles the rest.
Q3: I’m concerned that this will come across as too robotic and impersonal to my patients.
It’s all in the execution. A poorly written, generic email can come across as impersonal. However, a well-crafted message that uses the patient’s name, references their specific doctor and appointment time, and provides genuinely helpful information comes across as attentive and professional. Furthermore, by automating these routine communications, you free up your staff’s time to provide more personalized, high-touch service to patients who need it most.
Q4: How much does a system like this cost?
The cost of patient communication tools varies depending on the size of your practice and the features you need. Most are sold as a monthly subscription (SaaS model). While it is an expense, it should be viewed as an investment. Calculate the revenue you are currently losing each month from no-shows. In most cases, the monthly cost of an automation platform is easily covered by preventing just a handful of no-shows. The ROI is typically very high and very fast.
Q5: Can’t I just have my front desk staff send these emails from our office account?
There is a massive difference between manually sending emails and true automation. A proper automation system integrates with your scheduler and triggers messages in real-time based on events, eliminating the need for human intervention. This ensures 100% consistency and reliability. It also provides tracking and analytics that a standard email account cannot. Asking staff to send templated emails manually remains a time-consuming, unscalable, and error-prone process that doesn’t address the core efficiency issue.
Q6: How long does the setup and implementation process take?
The timeline can vary, but a typical implementation can take anywhere from a few weeks to a couple of months. The main steps include selecting a vendor, signing the BAA, performing the technical integration with your PMS/EHR, designing and writing your initial workflows, and training your staff. Working with an experienced partner like InvigoMedia can significantly accelerate this process and help you avoid common pitfalls, getting you to your goal of a more efficient practice much faster.